The Fourth P
The Secret to Paying for Mental Healthcare in Lean Times
Receive the relevant articles, news, and resources about the mental health industry in our country.
Connect your patients with a dedicated advocate who provides personalized navigation to the most appropriate mental health resources, and follows them throughout their mental health journeys.
If you’ve read my book, Healing: Our Path from Mental Illness to Mental Health, you know the main message: recovery requires the three P’s. True confession: this was not my idea. I first heard about the 3 P’s from Dr. Jonathan Sherin, who was then the Director of the LA County Dept of Mental Health. The 3 P’s: people, place, and purpose were his way of explaining the essential role of social support, the need for a safe and nurturing environment, and the importance of having a personal mission (or at least something to get you out of bed each day). The 3 P’s became my mantra when talking about how we need to reform mental healthcare. Not just increasing the workforce or improving access to evidence-based treatment, but focusing on people, place, and purpose.
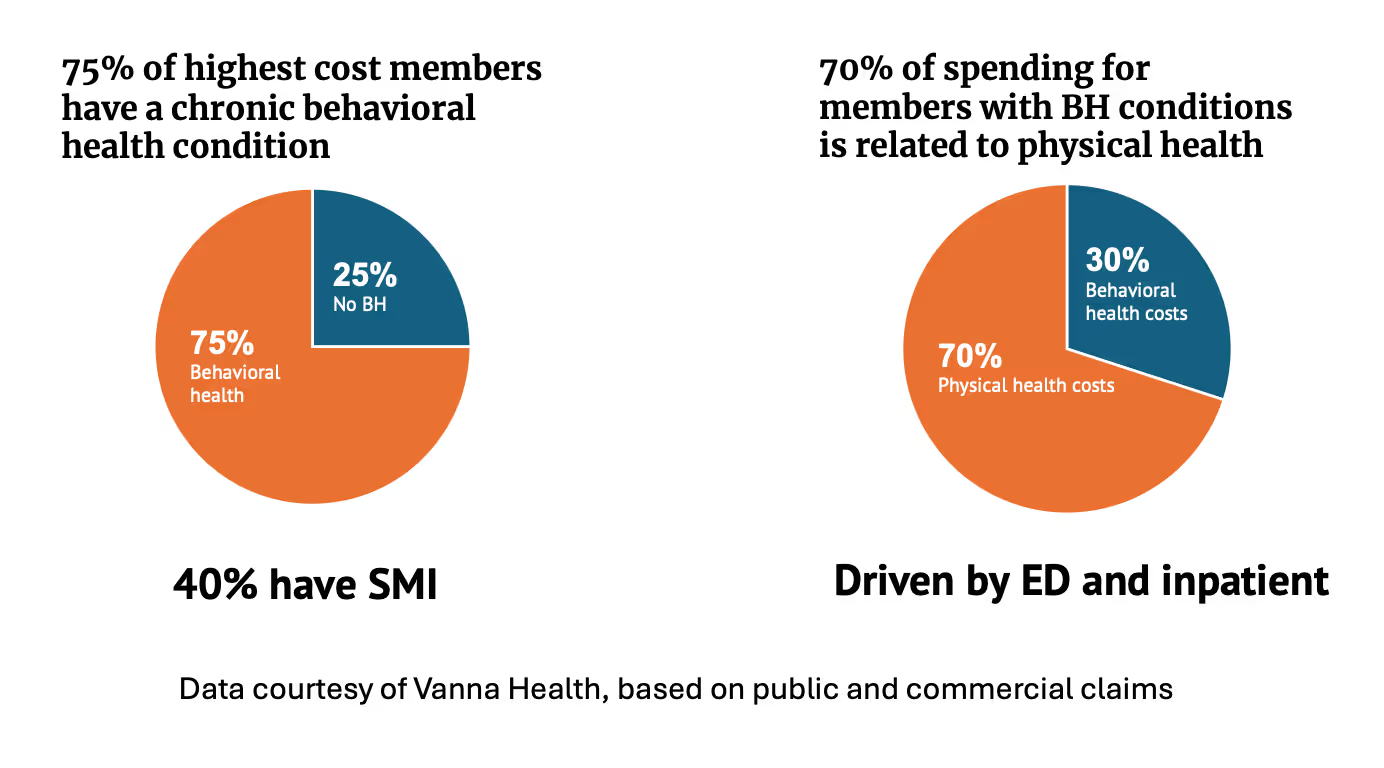
If these are essential for recovery, why don’t we deliver the 3 P’s? The answer is another P: payment. We spend a lot of money – over 17% of our GDP in the U.S. -- for healthcare. Focusing on the highest cost patients in our healthcare system, 75% have a behavioral health condition and roughly 40% have a serious mental illness. But of the nearly $5T we spend on healthcare, relatively little, roughly 6%, goes to behavioral healthcare. Most of the spend, especially for people with serious mental illness, is on physical health, neglecting treatment for the core problem. Emergency room visits and inpatient care drive much of these costs.
Of course, these are just the medical costs. The larger economic burden of serious mental illness is harder to capture but no less staggering: over $300 billion in lost productivity, a large fraction of our criminal justice expenses, and the incalculable impact on families with caregiving responsibilities and lost earnings. In short, the price of neglect is measured not just in ER visits and hospital stays, but in lost human potential, burdened families, preventable institutionalization, and early mortality. When we fail to invest in people, place, and purpose, the bill comes due in every corner of society.
So why don’t we pay for the 3 P’s? We know how to provide for people, place, and purpose. Clubhouses, community health workers, housing, supported employment – for decades, we have had a collection of services that have been proven to improve recovery and reduce costs. They cost a tiny fraction of an ER visit or an inpatient stay. In fact, they save money by pre-empting ER visits and inpatient stays. Yet, with rare exceptions, neither public nor private health insurance pays for these services.
It's a truism to point out that when we start to talk about health we too quickly talk about healthcare. Even though clinical care drives perhaps 20% of health outcomes, as a nation, we have decided that hospital systems and outpatient clinics and laboratory services define health care and thus are essential for health. Most of our innovation has driven greater use and greater costs of these services. But in the world of mental health, are these the right services for recovery? Are we spending too much by not paying for the 3 P’s? Can we use this fourth P (payment) to deliver the other 3?
With pending cuts to Medicaid, these questions have become urgent. Medicaid is the single largest payer for mental healthcare. The pending cuts will mean less care for people with serious mental illness. Like it or not, U.S. healthcare is a business. If an intervention isn’t paid for, it isn’t delivered. But maybe we don’t need to pay more; maybe we need to spend smart. Paying for people, place, and purpose is spending smart.
The clubhouse model is a great example. The clubhouse I know best, Fountain House in NYC, provides all three P’s: social support through an intentional community, a nurturing environment where people can spend their “work-ordered day”, and a sense of purpose through educational placements and job training. Beyond supporting thousands of people on their journeys of recovery, they estimate healthcare savings of roughly $11K per year per member, suggesting a savings of $700M at scale. You might assume that every state would use their Medicaid funds to support clubhouses. You’d be technically correct in 20 states. These states have allowed Medicaid funds to be used for clubhouses, but generally in 15-minute increments that reimburse so little that the economic juice is not worth the administrative squeeze. Ohio and California (as of 2025) have more reasonable rates but even in these states, clubhouses are under-resourced. Bottom line: as a nation, we do not support clubhouses with either public or private insurance.
As a business practice, a clinical practice, or a policy practice, our failure to support clubhouses is idiotic. While public and commercial payers struggle to cover intensive, expensive care, we fail to support affordable, effective alternatives. There are start-ups innovating on the 4th P for people with serious mental illness. I co-founded one of these, Vanna Health. And there are others – including First Hand, Amae, Flourish – that are proving out the economic value of focusing on the 3 P’s. These companies use community health workers and peers to demonstrate how less intensive, less expensive services can bring down the total cost of care while yielding better outcomes for people with serious mental illness.
James Carville, in a political campaign, famously noted, “It’s the economy, stupid.” As Dr. Sherin said to me, “It’s the 3 P’s that we need for recovery, stupid.” And the fourth P – payment – that we need to implement the other three. Now more than ever, we need to spend smart.
Take the first step toward better mental health today.
Ready to learn more about our Advocates? Reach out now and discover how our personalized support can guide you to the right mental health resources.


